Top 10 Lifestyle Changes to Lower Blood Sugar Naturally
Key Takeaways: Lowering Blood Sugar Naturally
Here's the quick rundown on what really works for getting your blood sugar in a better place.
- Move Your Body: Regular exercise, even short walks, makes your body use sugar better. Aim for about 150 minutes a week.
- Watch Your Carbs: Carbs turn into sugar. Focus on quality over quantity and learn portion sizes. The plate method is a great start.
- Eat More Fiber: Fiber slows down sugar absorption. Think vegetables, beans, nuts, and seeds.
- Drink Water: Staying hydrated helps your kidneys flush out extra sugar. Skip the sugary drinks.
- Sleep is Crucial: Poor sleep messes with the hormones that control blood sugar. Aim for 7-9 hours.
- Manage Stress: Stress raises blood sugar. Find what calms you down, whether it's exercise, meditation, or a hobby.
- Consider Meal Timing: Eating earlier in the day and trying things like intermittent fasting might help, but talk to a doctor first.
- Natural Supplements: Things like cinnamon or berberine can be a helpful addition to a healthy lifestyle, not a replacement for it.
Get Moving: How Regular Exercise Truly Changes Your Glucose Levels
So, how does moving your body actually help your blood sugar? It’s a bit of a two-pronged attack, really. First, when you exercise, your muscles need energy. They get this energy from the glucose that's floating around in your blood. The cool thing is, they can grab this glucose and use it up without needing much insulin to help. Think of it like your muscles having a VIP pass that lets them bypass the normal insulin process during a workout.
This immediately lowers the amount of sugar in your bloodstream. It’s a direct, almost instant effect. I’ve seen clients check their sugar before and after a brisk 20-minute walk, and they're always amazed at the drop. It's real, and it works. This isn't some complex biological process you need a degree to understand; its simple cause and effect. You move, your muscles use fuel, your blood sugar goes down.
The second part is more of a long-term benefit. When you make exercise a regular part of your life, your body becomes more sensitive to insulin. What does that mean? It means the insulin you do produce works way more efficiently.
Your cells are no longer ignoring its knock at the door. Instead, they open right up and let the glucose in, pulling it out of the blood where it can cause problems. This increased sensitivity can last for 24 hours or even more after a decent workout. This is why consistency is so much more important than intensity, especially when you're starting out.
A daily walk is better than one monster gym session a week that leaves you sore and unwilling to move for days. Don’t feel like you have to become a marathon runner overnight. The best exercise is the one you'll actually do.
Let's talk about what kind of exercise is best. Honestly, anything that gets your heart rate up a bit is fantastic.
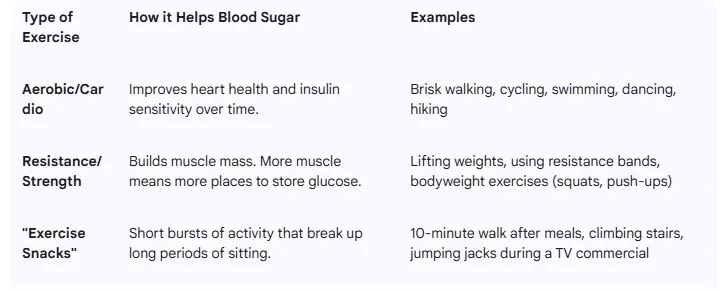
A lot of people get stuck thinking they need a full hour. They don't. Research has shown that even 10-minute bursts of activity spread throughout the day are incredibly effective. A short walk after breakfast, lunch, and dinner can have a massive impact on your post-meal blood sugar spikes.
A client of mine, a busy office worker, started just walking up and down the stairs at his office for 10 minutes a few times a day.
He didn't change his diet at first, just added this movement. Within a month, his fasting numbers were noticeably better. It's about breaking that sedentary cycle. Your body was made to move, and giving it what it needs pays off big time for your metabolic health.
Rethinking Your Plate: Smart Carb Choices and Portion Awareness

Managing carbohydrates is probably the most direct way to manage your blood sugar, since carbs are the food group that breaks down into glucose. But it's not about cutting out all carbs forever, that's just not sustainable for most peoples. It’s about being smarter with your choices. Your body needs carbohydrates for energy, but the type and amount make all the difference.
Think about it this way: a slice of whole-grain bread and a sugary doughnut might have a similar carb count, but they behave completely differently in your body. The doughnut causes a huge, fast spike in blood sugar, while the fiber in the whole-grain bread slows everything down, leading to a much gentler, more manageable rise. Focusing on low-glycemic index (GI) foods—those that are digested slowly—is a game-changer. These include foods like beans, lentils, most vegetables, and whole grains.
This is where portion control comes in, and it's not as tedious as it sounds. You don’t always have to weigh and measure every single thing you eat. One of the best tools I recommend to clients is the "plate method." It's visual and simple. Take your dinner plate: fill half of it with non-starchy vegetables. Think broccoli, salad greens, peppers, cauliflower, green beans. They're packed with fiber and nutrients and have a minimal impact on blood sugar.
Fill one quarter of the plate with a lean protein source like chicken, fish, tofu, or beans. Protein helps you feel full and satisfied and also helps stabilize blood sugar. Then, fill the last quarter with a high-quality, high-fiber carbohydrate. This is where your brown rice, quinoa, sweet potato, or whole-wheat pasta goes. Using this method, you automatically control your carb portion without having to do complex math.
I had a client who was so anxious about counting every gram of carbohydrate. It was stressing him out, which, ironically, can also raise blood sugar. I convinced him to drop the carb counting for two weeks and just use the plate method for his main meals. He was skeptical, but he did it. Not only did his blood sugar numbers improve, but his stress levels plummeted.
He realized he could manage his condition without it taking over his entire life. It’s about creating a balanced plate that balances your blood sugar. You’re not depriving yourself; you’re just re-prioritizing what's on your plate to give your body the right fuel mix. This approach is more intuitive and much easier to stick with long-term than a super restrictive diet.
The Power of Plants and Water: Upping Fiber and Hydration

Fiber is one of the most underrated heroes in the blood sugar story. Specifically, we're talking about soluble fiber. When you eat foods rich in it, this fiber forms a sort of gel in your digestive system. This gel slows everything down, including how quickly your body absorbs the sugars from your meal.
It prevents that sudden, sharp spike in blood glucose that you get from low-fiber, processed foods. Instead, you get a slower, more gradual release of energy. It’s a huge help for both type 1 and type 2 diabetes management.
The goal is to get around 30 grams of fiber a day, which sounds like a lot because most of us are only getting a fraction of that. But it's easier than you think if you focus on whole foods. Don't just run out and buy a fiber supplement; get it from your food.
Here's where you find the good stuff:
- Legumes: Lentils, chickpeas, black beans, kidney beans.
- Vegetables: Brussels sprouts, broccoli, carrots, artichokes.
- Fruits: Apples (with the skin on!), pears, berries, avocados.
- Whole Grains: Oats (not the instant sugary kind), barley, quinoa.
- Nuts and Seeds: Chia seeds, flaxseeds, almonds, walnuts.
Just by adding a salad to your lunch, switching to whole-grain bread, and snacking on an apple with some almonds, you can seriously boost your fiber intake. It makes you feel fuller for longer too, which helps with weight management.
Now let's talk about water.
It seems too simple to be true, but proper hydration is vital. When you're dehydrated, the glucose in your blood becomes more concentrated, and your readings can be higher. Drinking enough water helps your kidneys do their job, which includes filtering out and flushing away excess sugar through your urine. It's your body's natural detox system.
A study actually found that people who drank less water had a higher risk of developing high blood sugar. So how much should you drink? It varies, but a good rule of thumb is to drink enough so your urine is a pale yellow colour. And what you drink matters. Water is the perfect choice because it's zero-calorie and has no sugar.
Things like soda, sweetened iced tea, and even a lot of fruit juices will do the exact opposite of what you want, they'll send your blood sugar soaring. Stick with water. If you find it boring, try infusing it with some lemon, cucumber, or mint.
Your Nightly Reset: The Deep Link Between Sleep and Blood Sugar
Sleep isn't a luxury; it's a non-negotiable part of good blood sugar control. When you're sleep-deprived, even for just one night, your body goes into a state of stress. It releases more of the stress hormone cortisol, and one of cortisol's main jobs is to tell your liver to pump out more glucose to give you energy to deal with the perceived threat.
At the same time, sleep deprivation makes your body's cells more resistant to insulin. So now you have more sugar in your blood and your body is worse at handling it. It's a perfect storm for high blood sugar readings, especially in the morning. Many people with poor sleep habits notice their fasting blood sugar levels are stubbornly high, and this is often why.
There’s a vicious cycle that can happen here, too. High blood sugar can make you need to use the bathroom more often during the night, which interrupts your sleep. Then that interrupted sleep leads to even higher blood sugar the next day. It’s a loop that can be hard to break.
The goal is to aim for 7 to 9 hours of quality sleep per night. It’s not just about the hours you're in bed; it's about getting deep, restorative sleep. I always tell my clients that fixing their sleep can be as powerful as changing their diet. I've seen peoples' fasting glucose improve dramatically just by them prioritizing an earlier bedtime and creating a better sleep environment. It shows how interconnected our body's systems are.
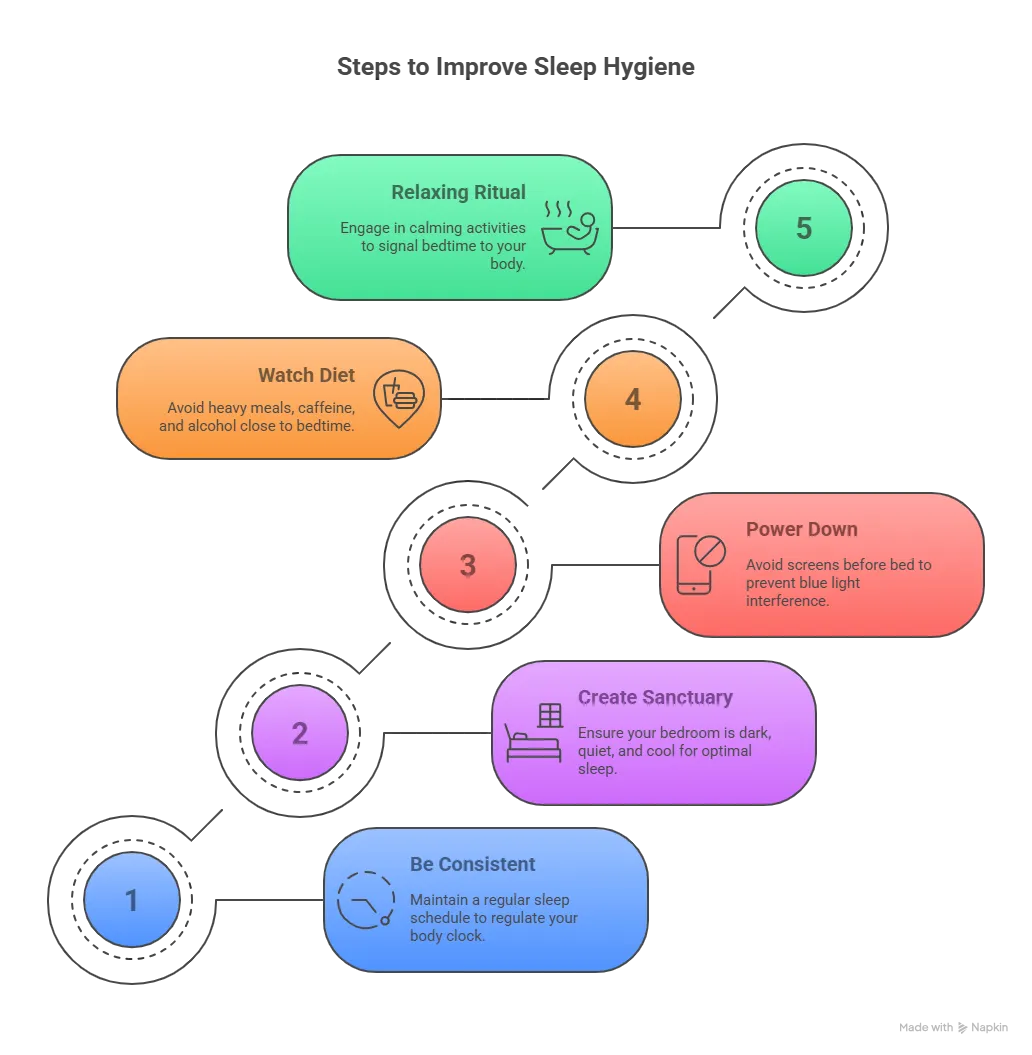
So, how do you improve your sleep? It comes down to good 'sleep hygiene.'
- Be Consistent: Try to go to bed and wake up around the same time every day, even on weekends. This helps regulate your body's internal clock.
- Create a Sanctuary: Your bedroom should be dark, quiet, and cool. Use blackout curtains or an eye mask if you need to.
- Power Down: The blue light from phones, tablets, and TVs can mess with the production of melatonin, the hormone that makes you sleepy. Stop using screens at least an hour before bed.
- Watch What You Eat and Drink: Avoid big meals, caffeine, and alcohol too close to bedtime. They can all interfere with your ability to fall and stay asleep.
- Create a Relaxing Ritual: Take a warm bath, read a book (a real one!), listen to calm music, or do some gentle stretching. This signals to your body that it's time to wind down.
Making these changes can take a little time to get used to, but the payoff for your blood sugar and your overall health is immense. Don't overlook the power of a good night's sleep.
Calm Your Mind, Control Your Glucose: Effective Stress Management
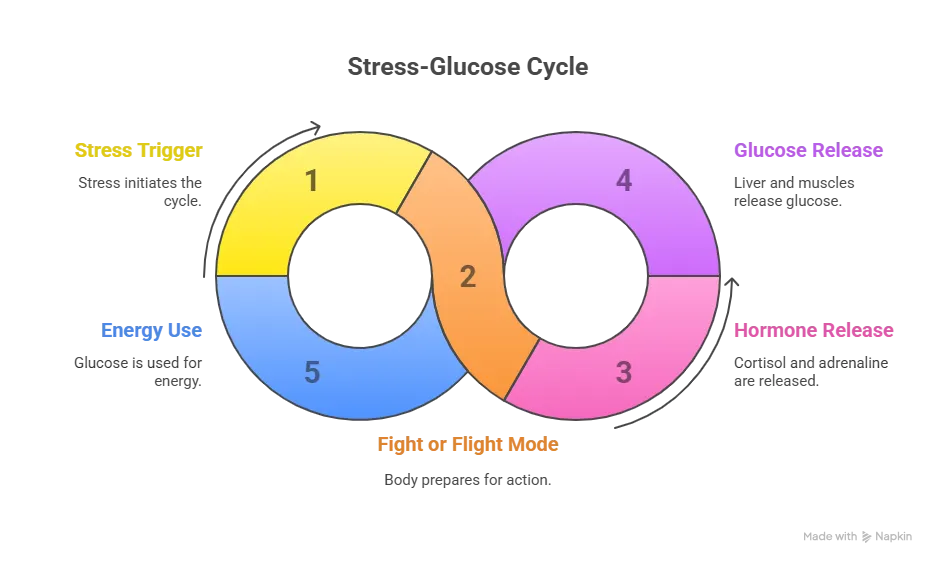
Stress has a direct, physical effect on your blood sugar levels. When you’re stressed, your body goes into “fight or flight” mode. It thinks it's in danger and needs a quick burst of energy to either fight off a predator or run away from it. To provide this energy, it signals your adrenal glands to release hormones like cortisol and adrenaline. These hormones tell your liver and muscles to release stored glucose into the bloodstream. In an ancient survival scenario, you'd burn off this extra sugar by fighting or fleeing.
But in the modern world, your "predator" might be a deadline at work, a traffic jam, or a family argument. You're not physically burning off that extra sugar, so it just stays in your bloodstream, pushing your levels higher.
The problem is particularly bad when stress becomes chronic, or long-term. If you're constantly stressed, your body is in a continuous state of high alert, and your blood sugar levels can remain persistently elevated. This makes it incredibly difficult to manage them, no matter how well you eat or how much you exercise. What's more, how do many of us cope with stress? We reach for "comfort foods," which are often high in sugar, unhealthy fats, and refined carbs.
This "stress eating" piles on even more glucose, making a bad situation worse. Understanding the connection between stress and blood sugar is the first step to breaking this cycle. You have to recognize that your mental state is directly tied to your metabolic health.
So, what can you do? You cant eliminate all stress from your life, but you can learn to manage it more effectively. The key is to find healthy coping mechanisms that work for you. Exercise is a fantastic one. It acts as a natural stress reliever and, as we've discussed, it also helps lower blood sugar directly. It's a win-win. Other powerful techniques include mindfulness and meditation.
You don’t have to sit cross-legged for an hour; even just five minutes of focused breathing can calm your nervous system and lower cortisol levels. Find a quiet place, close your eyes, and just focus on your breath going in and out. There are tons of free apps that can guide you through this.
Other strategies that people find helpful are spending time in nature, listening to music, engaging in a hobby you love, or talking things out with a friend or a therapist. I often advise clients to do a "stress audit." At the end of each day, take a few minutes to jot down what caused you the most stress. After a week, you can look for patterns.
Once you know your biggest triggers, you can make a plan to either avoid them or develop a specific strategy to cope with them when they happen. Maybe it's a 5-minute walk after a stressful meeting, or putting on your favorite song during your commute. Having a plan makes you feel more in control and less at the mercy of your stress response. Managing stress isn't a soft skill; it's a critical part of your blood sugar management plan.
Timing is Everything: Intermittent Fasting and Mindful Eating
Beyond what you eat, when and how you eat play a surprisingly big role in blood sugar control. Two powerful strategies here are intermittent fasting and mindful eating. Intermittent fasting (IF) has gained a lot of attention, and for good reason. It’s not a diet in the traditional sense, but an eating pattern. The most common method is the 16:8 approach, where you fast for 16 hours a day and consume all your meals within an 8-hour window. For example, you might eat between 12 PM and 8 PM and fast for the rest of the time.
Research suggests that this can improve insulin sensitivity and lower both fasting glucose and long-term markers like HbA1c. The fasting period gives your body a prolonged break from digestion and processing food, which can help reset its sensitivity to insulin. It can also help with weight loss, which further improves blood sugar levels.
However, a big word of caution is needed here. Intermittent fasting is not for everyone. If you are taking insulin or certain other diabetes medications, fasting without medical supervision can be dangerous and lead to hypoglycemia (dangerously low blood sugar). It is absolutely essential to talk to your doctor before trying any form of fasting to make sure it's safe for you and to figure out how to adjust your medications if needed.
It can be a great tool, but safety has to be the top priority. For some, especially students with hectic schedules, finding consistent meal times can be tough, but establishing some kind of routine is one of many healthy lifestyle tips that can make a big difference.
The second part of this equation is mindful eating. This has nothing to do with fasting and everything to do with your awareness during meals. In our busy lives, we often eat while distracted—watching TV, scrolling on our phones, or working at our desks. This leads to mindless eating, where we ignore our body's natural hunger and fullness cues.
Mindful eating is the practice of paying full attention to the experience of eating. You eat slowly, without distraction. You savor each bite, noticing the flavors, textures, and smells. You pay attention to your body and learn to recognize the physical signals that tell you when you're hungry and when you're satisfied. This practice helps you build a healthier relationship with food. It can reduce stress eating and prevent overeating, both of which are major contributors to poor blood sugar control.
It helps you get back in touch with your body's innate wisdom, which is something a lot of us have lost. Combining a structured eating window with a mindful approach during your meals can be a powerful combination for taking back control.
Exploring Natural Aids: Helpful Supplements for Blood Sugar
While diet and exercise are the cornerstones of managing blood sugar, some natural supplements have shown promise as helpful aids. I always stress to my clients that you cannot supplement your way out of a bad lifestyle. These are not magic pills. But, when used correctly alongside positive lifestyle changes, they can offer some extra support. Think of them as helpers, not heroes. Before starting any new supplement, its always best to talk with your healthcare provider, as they can interact with medications or might not be right for your specific situation. That said, some of the most well-researched options are worth knowing about.
Cinnamon is more than just a spice for your toast. Studies have suggested it can help lower fasting blood sugar and improve insulin sensitivity. It seems to work by mimicking insulin and increasing glucose transport into cells. Apple Cider Vinegar (ACV) is another popular one. Taking a tablespoon or two in a glass of water before a meal can help reduce the blood sugar spike from that meal.
Taking it before bed has also been shown in some small studies to lower fasting blood sugar the next morning. It's thought to improve insulin sensitivity or affect how the liver produces glucose. Then there’s Berberine, a compound extracted from several different plants.
This one is quite potent, and some research suggests its effects can be comparable to certain oral diabetes medications. It works on a molecular level to improve insulin sensitivity and decrease sugar production in the liver. Finally, Green Tea contains compounds like EGCG that can also enhance insulin sensitivity.
Here is a simple breakdown of these potential helpers.
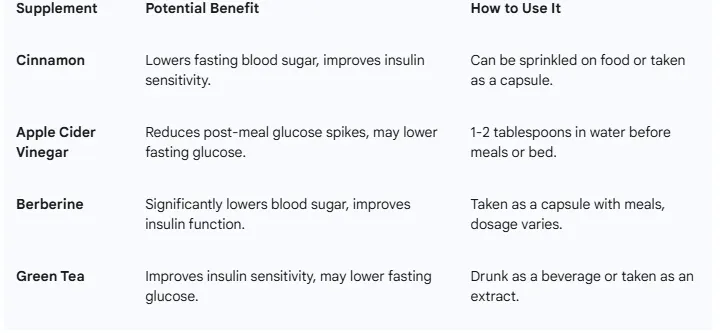
Again, these should be seen as part of a holistic plan. They work best when your diet is rich in fiber, you’re managing your carb intake, and you’re getting regular physical activity. If you're interested in learning more, you can find options to help optimize your blood sugar with these products. Just remember to approach them as a supporting actor in your health journey, not the main star. The real star is the consistent, daily effort you put into your lifestyle.
Putting It All Together: Your Sustainable Daily Routine
Knowing all these different lifestyle changes is one thing, but actually fitting them into your daily life is where the real work—and the real success—happens. The biggest mistake I see people make is trying to change everything all at once. They go from a sedentary lifestyle and a diet of convenience foods to trying to run five miles a day and eat nothing but kale. That approach almost always leads to burnout and a quick return to old habits.
The key to long-term success is to start small and build sustainable habits over time. The best plan is the one you can actually stick with, day in and day out. Consistency will always beat short-term intensity.
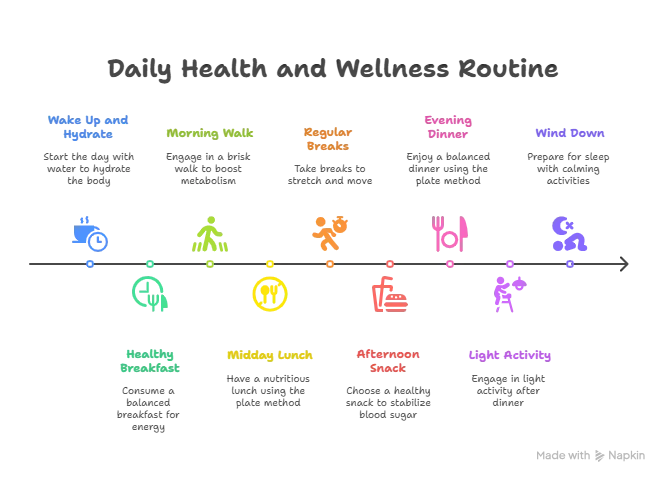
Let’s imagine what a day could look like, incorporating these changes in a manageable way.
- Morning: Wake up and drink a large glass of water to start your day hydrated. Instead of a sugary cereal, have a breakfast of scrambled eggs (protein) with spinach and a slice of whole-grain toast (fiber and quality carb). After breakfast, go for a brisk 10-15 minute walk. This helps your body handle the glucose from your meal and sets a positive tone for the day.
- Midday: For lunch, use the plate method. Maybe a large salad with grilled chicken and a scoop of chickpeas. Drink water, not soda. If you work at a desk, set a timer to get up and stretch or walk around for a few minutes every hour. This breaks up long periods of sitting.
- Afternoon: If you feel a snack attack coming on, reach for something that balances protein, fat, and fiber, like an apple with a handful of almonds or some Greek yogurt with berries. This will keep you full and your blood sugar stable, unlike a candy bar or a bag of chips.
- Evening: Use the plate method again for dinner. Perhaps salmon, roasted broccoli, and a small portion of quinoa. After dinner, do some light activity—maybe another short walk or some gentle stretching while you watch TV. An hour before bed, put your phone away. Read a book, listen to some calming music, or do a 5-minute guided meditation to manage stress and prepare your body for sleep.
This isn’t a perfect, rigid schedule. It’s a template. If you hate salmon, eat chicken. If you can't walk in the morning, walk in the evening. The point is to build a routine that integrates these principles in a way that feels good to you. Maybe your first step is just to add that 10-minute walk after dinner. Do that for two weeks until it feels automatic. Then, focus on changing your breakfast. By adding one small habit at a time, you build momentum.
Over a few months, you'll have completely transformed your routine without it ever feeling overwhelming. This is how lasting change is made. It's not about a dramatic overhaul; it's about a series of small, smart choices that add up to a healthier you.
Frequently Asked Questions (FAQs)
Q1: How quickly can I lower my blood sugar naturally? You can see short-term effects very quickly. A single session of exercise or a low-carb meal can lower your blood sugar within hours. For long-term improvements in things like your fasting blood sugar or HbA1c levels, it takes more consistency. You might see noticeable changes in your average readings within a few weeks of consistent lifestyle changes, with more significant improvements over 2-3 months.
Q2: Can I reverse prediabetes with these lifestyle changes? Yes, for many people it is absolutely possible to reverse prediabetes. By consistently applying these changes—improving diet, increasing physical activity, managing weight, sleeping well, and reducing stress—many individuals can bring their blood sugar levels back down to the normal range and prevent the progression to type 2 diabetes.
Q3: Do I need to give up all sugar and carbs? No, you don't need to eliminate all sugar or carbohydrates. The goal is to reduce added sugars (like those in sodas, sweets, and processed foods) and to choose your carbohydrates wisely. Focus on complex, high-fiber carbohydrates from whole foods like vegetables, legumes, and whole grains, and be mindful of your portion sizes.
Q4: Is fruit bad for my blood sugar? Whole fruits are generally not bad for your blood sugar when eaten in moderation. While fruit contains natural sugar (fructose), it also contains water, fiber, vitamins, and minerals. The fiber slows down the sugar absorption. It's much better to eat a whole apple than to drink apple juice, which has the sugar without the beneficial fiber. Berries, apples, and pears are great low-glycemic options.
Q5: When should I see a doctor about my blood sugar? You should see a doctor if you experience symptoms of high blood sugar, such as excessive thirst, frequent urination, unexplained weight loss, or extreme fatigue. It's also important to consult a healthcare provider before making any drastic changes to your diet or exercise routine, especially if you are already taking medication for diabetes or any other condition. Regular check-ups are always a good idea to monitor your blood sugar levels.